Claims processing is a critical aspect of the insurance industry, and yet it often poses significant challenges for companies. Extensive paperwork and complex procedures can lead to delays, inefficiencies, and ultimately, frustrated customers.
So how can you relieve this frustration and start creating claims experiences that customers love? The answer is through CX automation. Conversational apps are revolutionizing the insurance industry by streamlining the claims process.
In this article, we will share some real-life examples showcasing how some of the world's leading insurers have partnered with Hubtype to automate their claims processes. We will also explore the direct correlation between automation and improved customer experience.
The Benefits of Automated Claims Processing
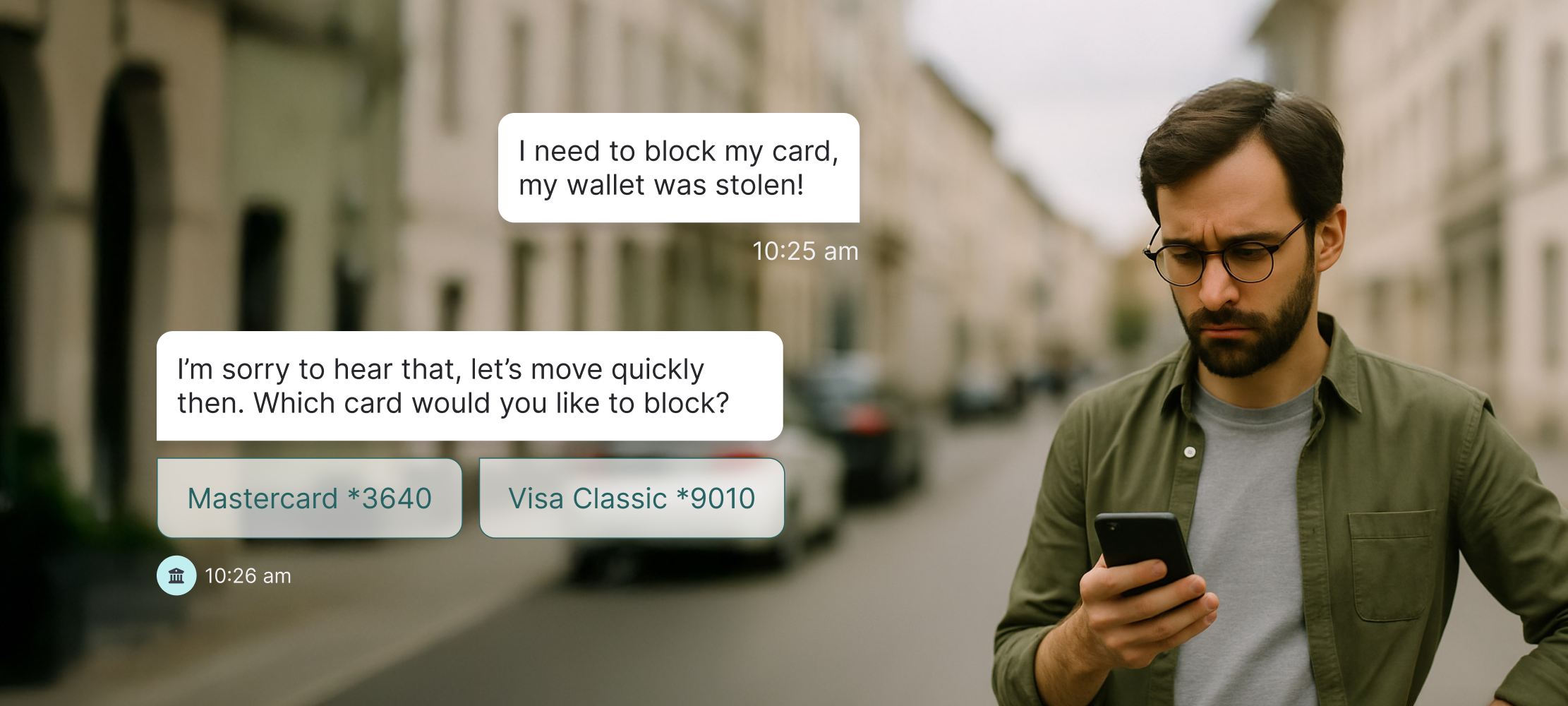
Picture this: A customer enters into your conversational app to begin their claims process. They choose the claim type, provide the necessary information and photos, and then submit the claim. All of this is completed in a matter of minutes and within the comfort of a single conversation.
Not only is automating the claims process faster and more seamless than ever, but also free of the time-constraints. Customers are able to make claims 24/7, without needing to wait for call center opening times or an agent to become available. Insurers who have automated their claims process with Hubtype have been able to resolve claims 5x faster, reduce contact center calls by up to 50%, and cut the overall cost of a claims journey by as much as 80%.
Since automated claims processing means real-time and asynchronous communication, this gives customers the flexibility and control over how and when they make their claims, and customers appreciate this. In fact, 75% of customers were more satisfied with automated processes because they provide instant responses.
Use Cases of Automated Claims Processing
Fast-track claims processing
Automated claims processing offers various benefits and use cases in the insurance industry. One key application is fast-track claims processing for low-risk and straightforward cases. By leveraging automated algorithms and predefined criteria, insurers can quickly process and approve claims that meet specific parameters. This streamlines the entire claims process, reducing the time it takes for policyholders to receive their settlements and increasing operational efficiency for insurance companies.
Expedited claims handling
In high-priority cases where time is of the essence, expedited claims handling becomes crucial. Automated systems can prioritize these cases based on predefined criteria, such as severity or urgency. By accelerating the processing of these claims, insurers can provide timely assistance to policyholders, especially in situations where immediate action is necessary, such as emergency medical claims or property damage claims following a natural disaster.
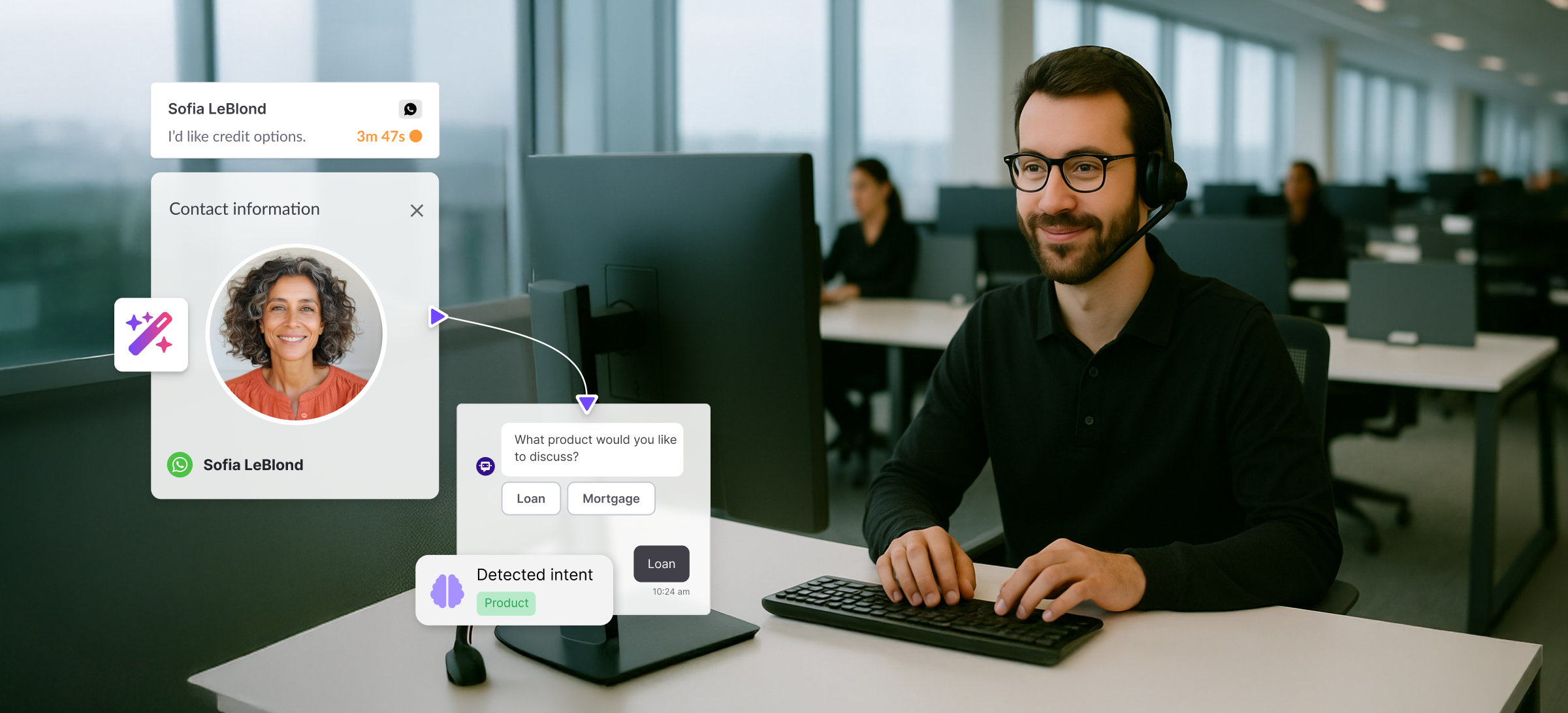
Intelligent claims routing
Furthermore, automated claims processing incorporates intelligent claims routing, directing each case to the appropriate departments or specialists within the organization. By analyzing claim details, such as the type of coverage and nature of the incident, the system ensures that claims are promptly routed to the right professionals who possess the expertise to handle them effectively. This intelligent routing enhances efficiency, reduces processing time, and improves customer satisfaction through a more personalized claims experience.
Streamlining the FNOL Process
First Notice of Loss (FNOL) is a critical moment in the claims process, often occurring under stressful circumstances. Automating this process through messaging apps like WhatsApp and Webchat can significantly improve efficiency and customer satisfaction. Customers can report incidents, upload photos, and provide necessary documents directly from the accident site, providing them with peace of mind. The automation system then uploads this data instantly to the claims system, reducing delays and errors.
Seamless integration with third-party services
Seamless integration with third-party services and data sources is a vital aspect of automated claims processing. By connecting with external systems, such as healthcare providers, repair services, or public records databases, insurers can obtain the necessary information and documentation to process claims efficiently. This integration enables automated retrieval of relevant data, such as medical records, estimates, or legal documents, saving time and reducing manual effort for both insurers and policyholders.
What does Whatsapp Automation look like in action?

A great example of how conversational apps can improve customer experience for insurers is this claims journey. This demo shows just how quickly a customer is able to make a claim on their car insurance.
Through this bot they are able to upload all the relevant information, as well as attach photos to their claim with just a few clicks of a button. Faster resolutions, and happier customers.
Start automating your claims processes
Automated claims processing using CX automation and conversational apps has proven to be a game-changer in the insurance industry. Hubtype's solutions have effectively demonstrated how this technology can save time, reduce costs, and enhance the customer experience for insurers.
With the continuous advancements in technology, the future of automated claims processing holds great promise for further optimization and improved efficiency. To fully explore the benefits of Hubtype's CX automation solutions in the insurance sector, book a demo with us today to start automating.

.jpeg)






.jpg)
